Syntetic Biology and Tissue Engineering Laboratory
Bioengineering and Chemical Engineering Department
The most common treatments used against cancer are surgical methods, radiotherapy and chemotherapy; the latter one of the most used in our country. Although these therapies are effective, in some cases they do not manage to completely eradicate cancer, and considerably wear down not only the patient’s immune system, but also his mood due to side effects.
Hopefully, in the last 10 years immunotherapy has made its way as one of the most suitable treatments for different types of cancer. Immunotherapy uses patients’ immune systems to attack cancer. One form of immunotherapy is CART-cell therapy, used to treat blood cancers such as leukemia, lymphomas, and myelomas. However, while CART-cells are optimal for identifying specific antigens in blood cells, they are not optimal for targeting tumors, as they are made up of different cells with different antigens on their surfaces.
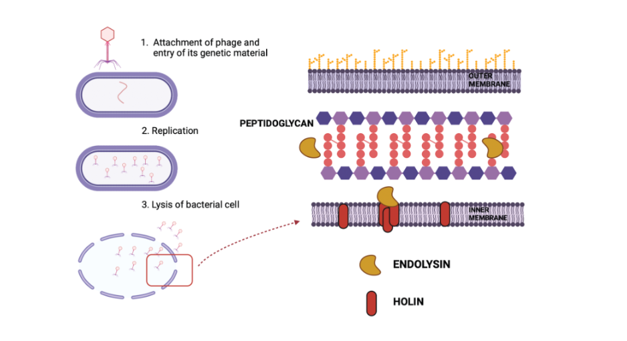
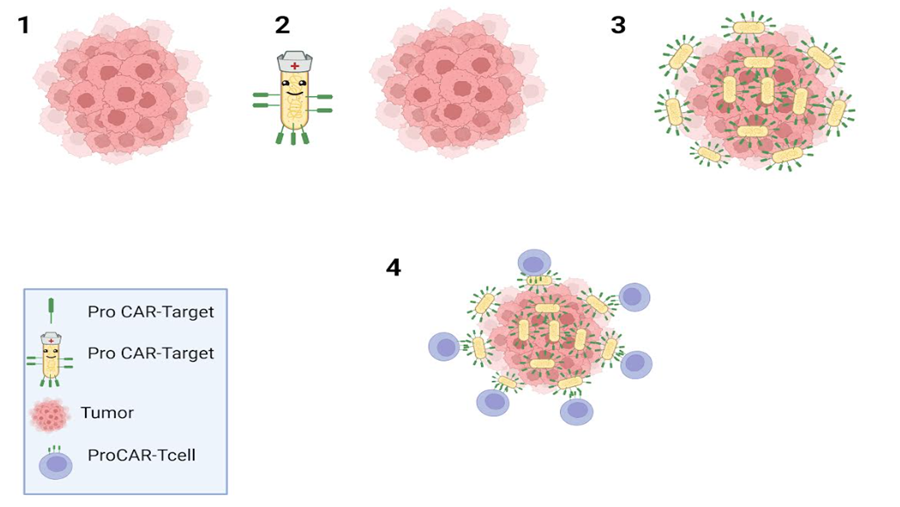
Faced with this problem, researchers from Columbia Engineering recently presented a novel strategy to combat tumors: they have modified probiotic bacteria to colonize tumors and thus generate synthetic targets within them, guiding CAR-cellsT to remove newly identified cancer cells. This new strategy marks the first time that genetically modified T cells are combined with altered bacteria to safely, systematically and effectively carry synthetic antigens to solid tumors. This approach could have a significant impact on the treatment of various forms of cancer.
The group of researchers led by Tal Danino, associate professor in the Department of Biomedical Engineering at Columbia University, has essentially developed a universal CAR-T cell designed to attack a universal antigen. This is achieved by programming tumor-seeking bacteria to mark solid tumors with a synthetic marker recognizable by CAR-T cells. Researchers anticipate that, with continuous refinements, This platform could treat any type of solid tumor without the need to identify a specific tumor antigen; consequently, it would not be necessary to create a customized CAR-T cell product for each cancer type and for each individual patient.
The creation of this platform of probiotic-guided CAR-T cells (ProCAR) represents an innovative achievement, and constitutes a first instance in which scientists have not only successfully integrated genetically modified probiotics with CAR-cellsT, they have also provided initial evidence that CAR responds to synthetic antigens produced directly within the tumor.
The platform has been shown to be safe and effective in several cancer models in humans and mice, encompassing both immunocompromised and immunocompetent mice. Notably, the study indicates that the presence of immunonestimulant bacteria within the tumor significantly improves the tumor removal functions of human T cells
All this said, and although the results are promising, it is necessary to wait for approval by the FDA as well as the large-scale implementation of this method; in order to avoid it becoming an excessively expensive treatment for patients.
Bibliography :
Rosa L. Vincent, Candice R. Gurbatri, Fangda Li, Ana Vardoshvili, Courtney Coker, Jongwon Im, Edward R. Ballister, Mathieu Rouanne, Thomas Savage, Kenia de los Santos-Alexis, Andrew Redenti, Leonie Brockmann, Meghna Komaranchath, Nicholas Arpaia, Tal Danino. Probiotic-guided CAR-T cells for solid tumor targeting. Science, 2023; 382 (6667): 211 DOI: 10.1126/science.add7034
Columbia University School of Engineering and Applied Science. “Engineered bacteria paint targets on tumors for cancer-killing T cells to see.” ScienceDaily. www.sciencedaily.com/releases/2023/10/231012161702.htm (accessed November 15, 2023).